Orthopectus : F.A.Q.
The deformities of the anterior chest wall are known as pectus carinatum or “pigeon chest” and pectus excavatum or “shoemaker chest”. They are very common, but remain hidden from society because people who have these deformities are usually ashamed of their chest aspect, avoiding clothing and activities that make these deformities noticeable. In 1990/91 Haje and colleagues conducted an experiment that resulted, for the first time in history of Medicine (see article), in reproduction of pectus deformities in animals, suggesting that these deformities occur due to a disproportion between the growth of the sternum (chest bone) and costal arches (costal cartilages and ribs).
Clinically, close to 5000 patients were observed by Haje from 1977 to March 2012. As pectus deformities are varied, and many times aesthetically different from each other, but with a common causal factor – disturbances in the formation and in the growth of the anterior chest wall bones and cartilages (see article) – such deformities can be considered a syndrome*. Common factors are involved in its pathogenesis: heredity, respiratory disturbances like bronchitis, asthma, pneumonia, rhinitis and sinusitis, spine mal-alignment like scoliosis and/or increased thoracic kyphosis, and a common psychological profile that aggravates with the adolescence growth spurt and the natural increase of the deformity due to the chest wall bones and cartilages disproportional growth. The psychological impact of a pectus deformity can be devastating on a patient and this impact is not always related to the severity of the deformity. Feelings of frustration can increase with medical suggestion to accept the deformity or just try a surgical solution.
*A syndrome is not a disease. A syndrome is a group or association of several signs and symptoms related to a same pathology, which together define the diagnosis and the clinical picture of a medical condition.
Nicolas Andry, the man considered the “Father of Orthopaedics,” in his book L’orthopédie ou l’art de prev’enir et de corriger dans les enfants, les difformités du corps, published in Paris in 1741, observed that limb deformities could be corrected through conservative methods of treatment. Later, Julius Wolff described what is accepted as a law in Orthopaedics: “The bone tissue is a dynamic structure that can be remodeled according to external forces.”
What we have been doing is using these concepts to correct pectus deformities. Despite being solid, bone and cartilage are live substances that have the capacity of remodeling. The younger the patient the greater is his/her potential for osteocartilaginous remodeling, but such a remodeling occurs throughout life.
Endochondral ossification and growth plates in the sternum and ribs are also concepts that have important implications for the correct approach to pectus deformities. We have paid attention to the fact that the bones and cartilages of the anterior chest wall also suffer the Wolff’s law effects, and that the flexibility presented in the chest allows the use of external forces to improve or cure a pectus deformity. Corrective forces can change the stress history of skeletal tissues to beneficially alter subsequent patterns of growth and ossification. So, we use external forces to modify the growth and promote the remodeling of deformed structures of the anterior chest wall. Such therapeutic options, based on orthopaedic principles, have been proven effective in patients with flexible deformities.
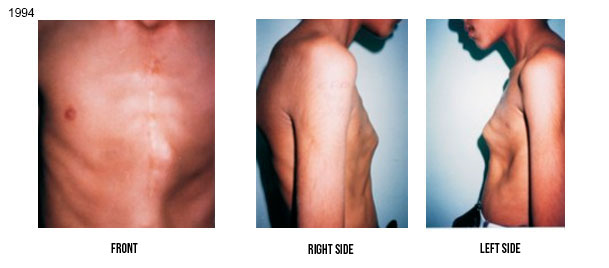
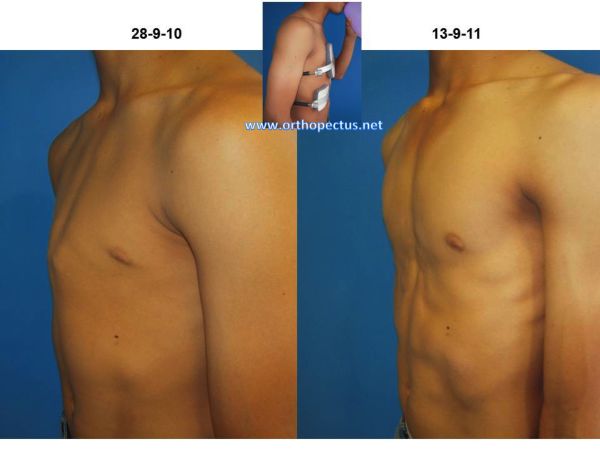
So, we use to combine external forces (orthoses) and internal forces (increased intrathoracic pressure due to the exercises while wearing the orthoses) to modify the growth and promote the remodeling of deformed structures of the anterior chest wall. Such therapeutic options, based on orthopaedic principles, have been proven effective, mainly in patients with flexible deformities. An example of such a remodeling is shown in the below Figure. The deformity of this patient occurred after cardiac surgery when he was 2 years old (see publication in our Bibliography section). He was treated by our method – orthosis + exercises – from 9 to 17 years of age (1994 to 2002).

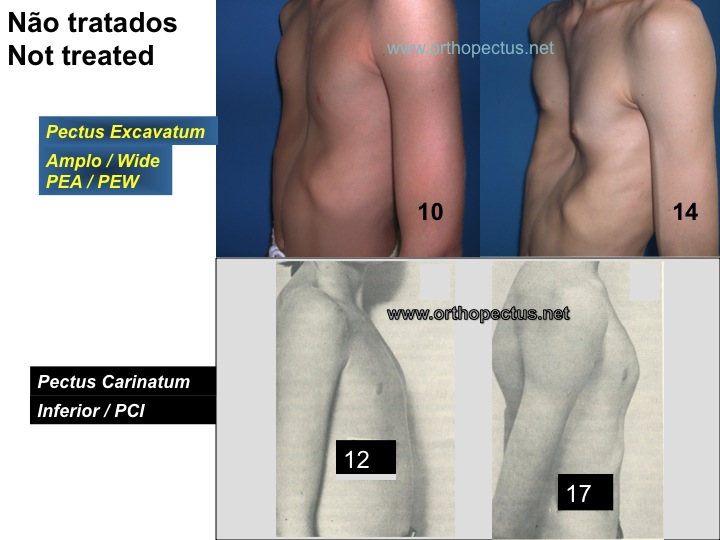
The vast majority of pectus deformities (99%) are IDIOPATHIC in nature, i.e., they occur without a previous pathology, being often associated with heredity. The two other less common forms of occurrence are the PATHOLOGIC, that occurs in the presence of diseases with growth disturbances in general, like Marfan’s Syndrome, bone dysplasias, rickets, osteogenesis imperfecta, etc, and the IATROGENIC, that may develop after medical action in pediatric cardiac surgery, due to lesion and anatomic disarrangement of the sternal growth plates. Usually there is no harm to internal organs, but psychic involvement can aggravate in adolescence. Pectus deformities left without treatment can get worse with the growth of the individual. Some examples of worsening of untreated deformities are shown below.

In the 1950’s and 60’s decades, surgery was reported as the only option of treatment for pectus deformities and any trial of conservative treatment condemned as ineffective. Doubts and critics about surgical results have occurred since the 70’s, with reports of complications of high morbidity such as wound infection, wound hematoma, pneumothorax, atelectasis, ugly scars, keloid, decrease in pulmonary function and death. Surgeons disagree about methods and modifications continue to be advocated. Reports on the existence of >40 different operative techniques raise suspicion that an ideal operation has not yet been devised. On the other hand, in 1969, Lange and Müller described some success when bracing with belts small children with pectus carinatum. Despite the fact that the sternum is attached to the spine by the costal arches, contemporary orthopaedics has paid attention almost only to the back part of the human trunk, i.e., the spine. Just in 1993 one case of a female pectus carinatum adolescent, successfully treated with plaster cast followed by bracing with belts, was reported by Mielke & Winter in the United States.
On the other hand, since 1979 Haje and coauthors have reported good results with a conservative treatment for pectus carinatum deformities, the ones with protrusion of the sternum, through a met hod that involves the use of an orthosis or brace, the Dynamic Chest Compressor (DCC). There are two orthoses variations: the DCC 1, normally used for pectus carinatum, and the DCC 2, that we have created in 1988 for pectus excavatum treatment. Mixed types of pectus (see next question) may require simultaneous use of a DCC 1 and a DCC 2. Appropriate exercises along with the orthoses (or braces) wear, are taught to the patient. We call this method of treatment as the Dynamic Remodeling method (DR method) and it is based on the bone remodeling law described in the answer of question 1. This approach is exclusively NON-SURGICAL! It is a CONSERVATIVE long term approach by the use of orthoses (braces) and exercises. It can lead to good or excellent results in one, two or more years, DEPENDING ON HOW THE PATIENT FOLLOWS APPROPRIATE INSTRUCTIONS (see PROTOCOL in question 14).
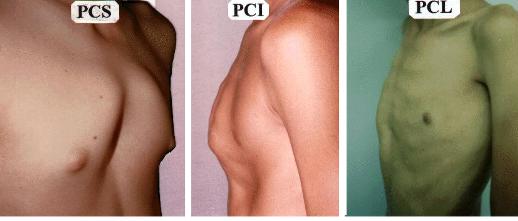
We classify the Pectus Carinatum, according to the apex of the protrusion, in three basic types: Superior (PCS), Inferior (PCI) and Lateral (PCL).
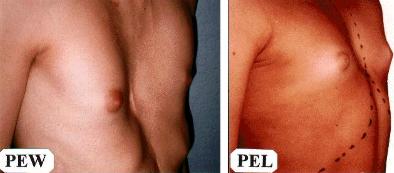
The Pectus Excavatum deformities, the ones with pure sternal depression, are classified into Wide (PEW) and Localized (PEL). (See figure below).
MIXED types, as PCL+PEL, PCS+PEL, PCL+PCS+PEL, etc, can also occur. Protrusion or flaring of the inferior ribs (close to the abdominal area) are also very common and illustrate the disproportional growth between the sternum and ribs (see causes of the deformities in answer of question
2).
Yes. The FLEXIBILITY of the anterior chest wall is more important than the severity of the deformity for prognosis of treatment using our method.
For assessment of the flexibility of pectus carinatum deformities, a manual compression test is done by compressing the protrusion area of the chest with the palm of one hand while the thoracic spine is supported by the other hand. If the protrusion decreases, it is still flexible.
For assessment of the flexibility of pectus excavatum deformities, an increased intrathoracic pressure test needs to be done as well. In a standing position, the patient takes a deep breath while actively contracts the abdominal muscles and holds the air simulating a blow to promote an increase of the intrathoracic pressure. Simultaneouly, the examiner manually compresses the bilateral flaring of the inferior ribs. The deformity is considered flexible if an improvement of the depression is noted.
Similarly to the orthodontic treatment, this is a long-term treatment and initial difficulties are expected. Nobody uses teeth devices for one or two months. So, the Dynamic Remodeling method for patients with pectus deformities can last one, two or more years, depending on the age, type and flexibility of the deformity, and mainly on how will the patient follow the medical instructions. In the first months or year we recommend wearing of the brace(s) as much as possible, including while sleeping. In this way the patient gets used to the presence of the brace and treatment progress is more efficient. As progress in treatment is observed and a stable correction noted, a gradual decrease in the brace(s) wearing, under medical supervision, is authorized. Complete interruption of treatment in a short period of time, without medical supervision, favors recidivism of a previously corrected deformity. On the other hand, the patient who does the weaning (gradual release) from the brace under a correct medical orientation obtains a stable and definitive correction. The improvement grade and the period of time to reach a stable correction depend on the way the patient follows the medical instructions. Example of an adolescent who began his treatment in January 2005 and was compliant to these rules for correct treatment, and who was free from the brace after 2 years and 8 months of treatment is shown in figure 9 of the section Treated cases of this site. The patient was completely released from any brace wearing one year and four months before the last photograph (Dec 08) and no recurrence was observed.
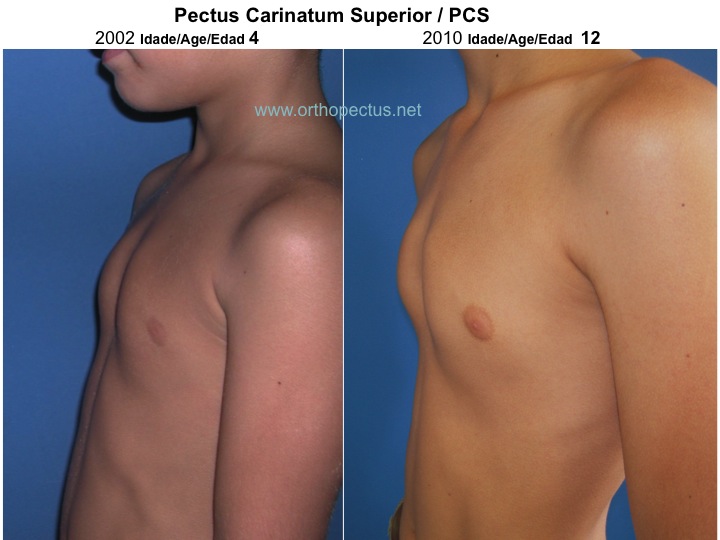
PCS: childhood. Other types of deformity: pre-adolescence or adolescence (see types of deformities in question 5). Pectus deformities are caused by disturbances in the formation and growth of bones and cartilages of the anterior chest wall and can get worse as the patient grows. See examples of worsening of each type of deformity without treatment, in different phases of the growing period, in question 3.
For PECTUS CARINATUM, usually the optimum period for starting our Dynamic Chest Compressor (DCC) orthoses is during the growth spurt of adolescence (from 12 to 14 years of age for boys or 11 to 13 for girls). Some cases can have the orthotic treatment started earlier, depending on the CLINICAL JUDGMENT about the severity and flexibility of the deformity, type of deformity and associated respiratory disturbances. We have observed improvement of respiratory disturbances, like Asthma, after treatment with DCC orthosis. Remodeling of the anterior chest wall in a beneficial way with the orthotic treatment seems to be responsible for such a breathing improvement. For the Pectus Carinatum Superior / PCS (see types of deformity in question 5), that usually presents a rigid deformity due to premature fusion of growing cartilages of the sternum (see example of PCS progression in CHILDHOOD in question 3) we ALWAYS recommend an earlier orthotic treatment, starting the use of a DCC orthosis or brace from 4 to 8 years of age. Only for a few cases of very severe deformities of all types of carinatum or mixed deformities we have started treatment around 3 or 4 years of age. A young child usually tolerates very well an orthosis constructed according to her deformity. An original orthosis usually lasts for two or three years (adjustments are usually required). With the growing of the child a new orthosis may be necessary. If deformity recurs in adolescence, a new orthosis, adapted to the residual deformity, will have to be worn again.
For very young children with PECTUS EXCAVATUM, blowing balloons and back-stroke / free style (crawl) swimming are recommended for keeping or improving the chest flexibility. For infants with Pectus Excavatum and flaring of the inferior ribs, passive exercises through digital intermittent pressure on the flaring of the ribs may help. – P.S. Digital pressure means pressure made by the thumb(s). Intermittent means occurring at short time intervals; having periods of cessation of activity (every 5 to 10 seconds). The pressure of your thumbs on the flaring of the ribs should be enough to depress the flaring. You can repeat the intermittent pressure as many times as the child tolerates. Usually about 10, 20 or 30 times everyday day are OK. The best moment to do that is after the bath, while you dry the child and make jokes with her.
For PECTUS EXCAVATUM we have seen the best results when our complete treatment (orthosis+exercises) starts in pre-adolescence and continue through adolescence. Learning how to blow a straw to make bubbles on a liquid is an important step in helping the very young child to acquire the blowing ability. The goal is to keep or improve chest wall flexibility until the adolescence or until the period the patient will start the orthosis (brace) wearing. The results for pectus deformities are not immediate and demand persistence from the patient, beside experience from the attending physician to conduct the orthotic treatment in a long period of time.
The Centro Clinico Orthopectus can see your child at any age. If the complete treatment (orthosis+exercises) is not recommended yet we can prescribe exercises appropriated for the patient’s age. Based on our clinical judgment after physical examination clinical photographs of the chest are taken for follow-up and start of the treatment at an appropriate age. The indication for orthotic treatment can happen in the first visit.
We do not recommend surgery for young children due to the risk of lesion to the sternum and/or ribs cartilaginous growth plates. Secondary growth disturbances and recurrence are common after surgery.
The following reports are also found in the medical literature: “More than 40 different operative techniques have been described to deal with Pectus Excavatum” (Isakov et al) “indicating that an ideal method has not yet been discovered”(Haje). “Operative techniques are controversial and a perfect result is not obtained with every procedure” (Heydorn et al). “Surgeons who recognize increasingly poor results as their patients grow older, blame the technique and seek a better one” (Humphreys and Jaretzki). “Bad results occur in children who are operated on before they are 12 years of age” (Milovic and Oluic) and “a poor long term outcome” (Ellis, Humphreys and Jaretzki) have been reported without any explanation of why these failures occur (see first example below). “Current surgical methods do not refer to the GROWTH PLATES of the sternum and costal cartilages, and operation may produce secondary growth disturbance…” (Haje). Reports on other complications after surgery, as a decrease in pulmonary function, exist in literature.
Yes. The flexibility tests need to be performed. If the deformity has some flexibility, it can be treated by the Dynamic Remodeling (DR) method. Only 5% of our treated patients are adults (we started treating adults from 1998/99). It is more difficult to follow the DR method in adult life, but not impossible. The gradual external force from a DCC orthosis on sternal or costal protrusions plus the increase in the intrathoracic pressure from the exercises on depressed areas in a long period of time results in a remodeling therapeutic process similar to the one observed in orthodontic treatments. In the past only children and adolescents were seen wearing orthodontics devices. Nowadays many adults wear them. Similarly, in the past we used our DCC orthoses only in children and adolescents, but with time some adults decided to try them, with good results. We always explain to adult patients, especially those with RIGID deformities, that if they want to try the orthotic treatment, a lot of effort and will power will be necessary. We have a surprising case of a 49-year-old male patient with PEL who was under treatment for over a year. He sent us an e-mail saying that he went thru a somewhat painful transformation, but which “cleaned” the frustration, the negative emotions and the prejudice of his past, making he feel as if he was “born again”. Some sacrifice seems to be necessary for an adult to follow the routine of the orthotic treatment + exercises, but when this happens, the patient really feels rewarded. At the end of the section ‘Treated Cases’ in our site, you can see examples of results of our treatment to some adults who had a lot of will power. The testimony of an adult patient can also be found in ‘Video/Testimony section’ of this site. Usually, most adults deformities are not very flexible but, by following the instructions, the patient first gains flexibility and, after some months or years, improvement of the condition. The younger the adult the better. Our success rate for adults is 27% (good or excellent results). That means 27% of our adults patients are compliant patients. Our success rate (good or excellent results for adolescents is 62%. We believe the reasons for a smaller success rate in adults are the smaller chest flexibility and bone remodeling capacity, beside social and professional commitments that imply in less brace(s) time wearing.
Some skin rash where the pads make pressure usually occurs during treatment. The intensity of skin rash varies from patient to patient. Wearing the brace over a clean T-shirt or using removable clean covers made of cotton jersey over the pads decreases the intensity of the rash. Topic medicine may eventually be required but should never be left under the pads. After some hours, remove the medicine with alcohol before wearing the brace again. Eventual skin marks go away with time at the end of the treatment.
Overcorrection, a serious complication, can also occur during treatment and should be controlled by an adequate medical supervision. Overcorrection is more common to occur in pectus carinatum, but it can also occur to flexible pectus excavatum deformities (see article).
For adolescents and adults with pectus deformities we prescribe exercises therapy only along with the use of DCC orhoses or braces. Exercises alone, especially the ones that increase pressure inside the thorax, like sit-ups, push-ups and weightlifting, without the use of a DCC orthosis/brace, can increase and/or make more rigid the pectus deformity. Muscles developed by the exercises may hide a little the pectus carinatum protrusion, but the deformed cartilages and bones are not corrected by the exercises alone, and the exercises usually bring more rigidity to the protrusion. For the pectus excavatum deformity exercises alone usually provoke a hypertrophy of the pectoral muscles increasing the central chest depression appearance.
The only exercise we can recommend for patients that we have not seen is swimming. Although swimming by itself can not correct a pectus deformity, it usually does not increase the rigidity or worsen the condition of the deformity. We recommend swimming only in the following styles: backstroke (50%), crawl (30%) and breast (20%). Our advice is to avoid the butterfly style, because we believe the direction of movements of this style may aggravate a pectus excavatum deformity and/or an increased thoracic kyphosis.
The DCC correctly built does not interfere with breathing. Indeed, we have observed that patients with respiratory problems, like asthma, improve their clinical condition with treatment progress by the Dynamic Remodeling method (DCC braces + exercises).
You must take the DCC brace off for bathing, for swimming and for playing sports that involve physical contact. You can also take it off for special occasions/parties. You have just to remember to put it on as soon as any of these activities is over. Remember that the longer you stay without it, beyond the recommended time for each stage of treatment, the longer the total treatment period. HAVE ON MIND THAT THE TREATMENT PERFORMANCE IS A PATIENT’S RESPONSIBILITY. THE PHYSICIAN’S ROLE IS TO PROVIDE THE PATIENT WITH CORRECT INSTRUCTIONS, BASED ON HIS PERSONAL EXPERIENCE. It must be considered that any strange object on the body may bother for some time until the patient gets adapted to it. Adjustments and repairs as treatment progress are usually necessary for comfort and efficiency.
The simple prescription of a brace by the doctor and the use of it without rules by the patient do not mean that a pectus deformity is being treated. The following treatment PROTOCOL must be followed:
1. to make customized DCC braces, according to the deformity type, from previous plaster cast mold, under medical supervision and detailed prescription for pads size and shape;
2. to explain to the patient that compliance is essential and that it is a long term treatment, with medical supervision and gradual weaning/release from the brace, in ONE, TWO or more years (the total treatment time depends on the deformity flexibility and, mainly, on how the patient will follow the instructions);
3. to take and save clinical photographs from similar angles, before, during and after treatment;
4. to make medical follow-up every two, three or four months (follow-up by email can eventually be done if initial clinical photographs and patient’s data are saved in proper files);
5. to make adjustments in the orthosis or manufacturing of a new one when necessary;
6. to prescribe exercises, always along with the wearing of the DCC orthosis(es), aiming no muscle hypertrophy, but to provoke movements that will result in inner (intra-thoracic) pressure increase on the anterior chest wall;
7. to make an interdisciplinary effort – physician (coordinator of the process), orthotist and physical therapist.
Yes. It is possible. In some cases can make the results even better. In Centro Clínico Orthopectus we also advice what is the best model of Vaccum Bell that the patient can use associated with our treatment method in patients with pectus excavatum. We have the 5 different test models of Vaccum Bell in our clinic to test the best one for the patient. We do not sell the Vaccum Bell.
Yes, I believe so, but the simple purchase of an appliance will not solve the patient problem because an adequate medical supervision is essential. Unfortunately, our method of treatment is still not well understood by other physicians, especially for pectus excavatum deformities. He have already seen many patients who received an inappropriate brace for treatment, sometimes making the deformity worse. They simply received a prescription for an orthosis that was built the way the orthotist wanted and used by the patient without previous clinical photograph, without rules or exercises practice. The shape and the correct pads placement is essential: see below examples of different DCC orthoses, built for the same type of deformity (PCI), one incorrect and the other correct. It is necessary that physicians follow our protocol for a successful treatment (see question 14). The use of screws is mandatory for a Dynamic Chest Compressor (DCC) brace; velcro straps or other ways of lateral closing, as clipping, do not work as a dynamic way of compression. The prescription of exercises along with the brace wearing should be made according to the skeletal maturation of the patient.

We must see the patient to better help him (or her). We have already treated without surgery hundreds of patients who came from all parts of Brazil, a country almost as large as the United States of America, and from other countries like Canada, England, the USA, Australia, Costa Rica, Colombia, Norway, Spain, Austria, Finland, Israel, Republic Dominican, Ireland, Macedonia, Uruguay, Italy, Germany, Slovenia, Portugal, Scotland, Japan, Argentina, Sweden, Denmark, Romania, Peru, Malta, Hong Kong, Ecuador, Chile, China, Mexico, Venezuela, Poland, Paraguay.
The period of time between the first and the last medical visit is usually around FOUR WEEKDAYS. You should arrive on a Sunday or Monday morning. The plaster cast mold is made in the first visit, Monday afternoon. One or two days are necessary for construction of the brace and two more days for exercise teaching sessions and final medical check for brace(s) adjustment(s). You could leave on Friday or Saturday of the same week. The initial stages of the treatment are: 1. first consultation and, if there is indication for immediate treatment, a cast mold of the thoracic deformity is made; 2. the orthosis (brace) is manufactured based on the mold and on detailed medical prescription according to the patient’s deformity; 3. visit for receiving the brace and instructions on how to use and take care of it and prescription of appropriate exercises; 4.practice of therapeutic exercises in use of the orthosis under the supervision of a properly trained physical therapist (a list of the exercises is given to the patient); 5. periodic revisions, every two or three months for the patient who lives nearby; for the patient who does not live nearby, or who lives in other country, but who had treatment initiated in the Centro Clinico Orthopectus, instructions for an adequate maintenance of the treatment can be given by email, until a revision visit can be done. Physicians from the patient’s town/country can provide a parallel follow-up of the case, as we are always prompt to clarify doubts if the patient has pre-treatment clinical photographs and data in our files, avoiding inappropriate changes in medical conduct.
Our clinic is located in Brasília, the modern capital of Brazil in South America. It is located in the center of the country, about 1000 km away from Rio de Janeiro and São Paulo, the most known cities of Brazil (about one and a half hour flight from each one). Nowadays, travelling abroad is not complicated and sometimes even cheaper than travelling in your own country.
Below are some observations done by one of our patients, a young woman who came from Canada by herself.
Some people at the airports in Brazil speak very good English, shop attendants do speak a little English, those who do not speak any English always try to find someone who does it; you can manage to do many things by yourself based on a Portuguese phrase book and by guessing similar words (retorno/return, hamburguer/hamburger, restaurante/restaurant, etc); Brazilians do use a lot of written words in English (sale, hot dog, milk shake, shopping, etc). Taxis are everywhere, about the price of those in the USA or Canada. Hotels and Shopping-Centers/Malls shops accept main credit cards like Visa, Mastercard, American Express, etc. . Street’s shopping-stands (fairs), taxis, cinemas, etc. only accept cash. Dollars or Euros can be exchanged by Brazilian currency (Real) at the airport, in banks and hotels. Brazilian people are very warm hearted and friendly. In Brasília you can go sightseeing, shopping, swimming, jogging, watch cable TV, etc. Clothes are fashionable and not very expensive. The weather is nice, around 23ºC; it gets hotter, up to 28ºC, in summer (Dec-March) and colder, around 14ºC, in winter (May-Aug), specially at night; it is very dry from June to September and sometimes very wet during summer time. By searching a website regarding travelling in Brazil you can find out almost anything you want to know.”
Appointments can be scheduled by e-mail. If you need information about how to organize your trip to Brazil, please contact the manager of our clinic, Mrs. Karla Haje, phone +5561 91078158 (day time) or +5561 32486292 (from 10:00 to 11:00 PM, Brazilian time), e-mail [email protected] and/or [email protected] She can help you book a hotel and give information on transportation services in Brasília. We make sure you are well assisted.
For those who are interested in receiving our knowledge in their own city we can give lectures, in English or Portuguese, and provide a four-day training with start of treatment in patients previously selected by local doctors. The focus of such activities is to train doctors, orthotists and physical therapists in their institution. In this case, the local medical service must support the training with cast room, orthopaedic workshop, material, orthotists to manufacture the orthoses and physical therapists to learn and teach exercises for the patients. All details must be worked out by e-mail [email protected] or [email protected], six months in advance.
“WE DO NOT SELL BRACES. WE PROVIDE A TREATMENT METHOD. THE ORTHOPAEDIC NATURE OF PECTUS DEFORMITIES MUST BE CONSIDERED!”



